
Warning: This article contains graphic images and discussion of eating disorders which some readers may find distressing.
A British woman was mistakenly diagnosed with an eating disorder after spending her teenage years battling undiagnosed Crohn’s disease.
Crohn’s disease, a long-term inflammatory bowel disease that currently cannot be cured, causes repeated flare-ups of symptoms including diarrhoea, stomach pain, anal pain, weight loss and blood or mucus in stools.
Lucy Dare, 21, first started experiencing symptoms of the condition when she was just 12 years old, with the initial signs including rectal bleeding, severe abdominal pain, weight loss, fatigue, using the toilet up to 15 times a day, and difficulty eating.
Advert
At the time, neither she nor her doctors knew what was going on, leading to Lucy's illness going undiagnosed for years.

The then-teen missed out on two years of school and could not sit her GCSEs as her symptoms left her anxious about leaving the house, needing the toilet at school, experiencing severe abdominal pain and being unable to eat.
At 13, Lucy weighed just 38kg, leading doctors to initially think she was experiencing an eating disorder.
This, on top of symptoms like needing to use the toilet urgently after mealtimes, led medical professionals to believe she had anorexia or bulimia.
"They thought it was an eating disorder, because I was 38kg," she said.
"Because I was such a low weight, and a young girl, they just assumed it was an eating disorder. They admitted me into an eating disorder unit, for six months to stay away from home."
"It was really horrible," Lucy added.
"There were girls in there self-harming, ripping tubes out, getting restrained, and I was just there in pain. I was confused about what was going on, why I was there, because I didn’t feel how they felt."
She spent six months as an inpatient at an eating disorder unit near her North London home. However, as symptoms hadn’t improved by the end of her stay, she was referred for an endoscopy and colonoscopy to explore the possibility of a physical illness.

It wasn't until 2019 that Lucy had a colonoscopy, which diagnosed her with Crohn’s disease.
She was prescribed infliximab and azathioprine, and put on the Modulen liquid diet to give her bowel a rest, so she couldn’t eat for six weeks – including her Christmas dinner.
After spending nearly a year in the hospital and the eating disorder unit, Lucy was able to get a weekend job in a hairdresser's. Following her first shift, she finally felt up to going out to see her friends, and she went for food at a local restaurant before going to her friend’s house for the evening.
Not long after arriving at her friend’s house, however, Lucy started having excruciating pain in her abdominal.
She recalled: "Suddenly, it just came on.
"I rushed to the toilet. I was just going to the toilet and vomiting non-stop, just really coming out. I couldn’t walk or anything.
"My mum had to come over to my friend’s house, pick me up and bring me down the stairs to go to A&E. Then they admitted me."
For the first two days of her hospital stay, Lucy was told that since doctors couldn’t hear any unusual sounds from her stomach, it was likely 'all in your head', and perhaps it was food poisoning causing her sickness.
"My mum was like, 'No, there’s something wrong. You need to do a scan, she’s not OK'," she said.
Lucy’s vomit was brown, which turned out to be faecal matter from her bowel, and her diarrhoea was a 'luminous green' colour.
Her mother, Leza was concerned that her bowel had perforated and that she was experiencing a severe infection known as peritonitis and urged doctors to conduct a CT scan.
The CT scan did confirm that Lucy’s bowel had perforated, a life-threatening condition where a hole forms in the intestine, allowing intestinal contents to leak into the abdomen, and she was immediately rushed into emergency surgery.
Lucy was told that following the surgery, she’d wake up covered in tubes and may even have a stoma – a surgical opening in the abdomen that allows bodily waste to be diverted into a stoma bag – and it was at this point that fear truly took hold.
She recalled: "I was staying strong, but once they started saying all of that, that’s when I was scared, like, really scared.
"And then I just burst out crying."

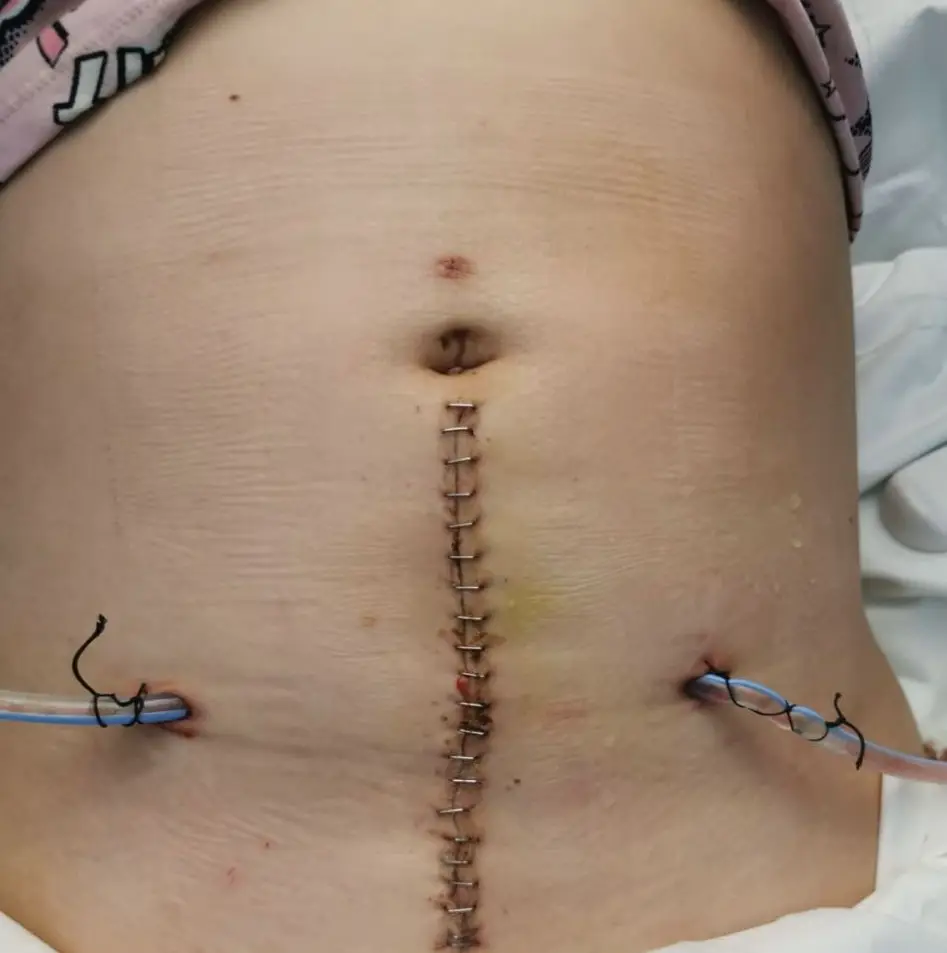
Unfortunately, Lucy wasn’t able to have a stoma due to the location of the surgery, but during the five-hour operation, 60cm of her small intestine was removed.
"I remember waking up in the ICU with tubes everywhere. I was so uncomfortable. I was really swollen," she said.
"I was left to the point where I was actually dying to get any sort of help. If they sent me home the weekend my bowel perforated like they tried to, I would have died."
Thankfully, Lucy was discharged just before the Covid-19 pandemic took hold, so she was able to be with her mum and not be isolated in hospital. However, recovery was far from easy.
"The recovery was hard, and it was long, just a long time of being uncomfortable and in pain," she said.
Five years on, and Lucy still has a long road ahead.
"It’s just been a lot of ups and downs," she explained. "I did have a job last year, but I lost it because I kept having time off all the time for Crohn’s. So I haven’t been able to work or anything."
She hasn’t been able to work and is currently deemed ineligible to claim personal independence payment (PIP), struggles to leave the house due to her pain and anxiety, and is trying a variety of medications in the hopes that one of them will give her some relief.

"Since starting treatment, things have actually got worse," she shared, though she noted that fitness, which she documents through her Instagram @liftwithlucyyy, 'gives me clarity, control, and a sense of strength that the illness often challenges'.
Lucy's last flare up was pancolitis in 2024.
"The whole of my large intestines was inflamed," she said, adding that last Sunday (28 November), she had a duodenoscopy and doctors diagnosed gastritis, so she is now waiting for the next steps.
Lucy and Leza feel it is essential to raise awareness of Crohn’s disease, and help stop other people from facing the battle Lucy fought to get a diagnosis.
"We hadn’t even heard of Crohn’s before Lucy," Leza said.
"A lot of people, a lot of girls, especially, I think, they get misdiagnosed with eating disorders. And it’s wrong. Obviously, periods as well, they put a lot of things down to that and body image, [being told] it’s in your head.
"And then you get left, and then it gets worse."
Pearl Avery, IBD Nursing Lead at Crohn’s & Colitis UK, said: "Although Crohn’s and Colitis can strike at any age, you’re most likely to be diagnosed when you’re young.

"That’s a lot of lives put on hold – days off work and school, plans cancelled and time spent in hospital when you should be out there getting on with your life.
"Unfortunately, Lucy’s not alone in having had to wait a long time for a diagnosis – for a quarter of those with Crohn’s or Colitis it takes over a year to figure out what’s really going on. Lucy knew there was something wrong and pushed for answers."
Pearl added: "But at Crohn’s & Colitis UK we’ve just done a poll which told us that over half of young adults either don’t know much about Crohn’s and Colitis or have never heard of the conditions at all.
"So, if you’re reading this and you’ve had blood in your poo, agonising stomach pain, unexplained weight loss and frequent, urgent diarrhoea, for example – visit the symptom checker on the Crohn’s & Colitis UK website and go to a doctor.
"Don’t let embarrassment stop you from seeking help. The sooner you find out what’s going on, the better."
You can find out more about Crohn's disease on the official NHS website here.
If you've been affected by any of the issues in this article and would like to speak with someone in confidence, call the BEAT Eating Disorders helpline on 0808 801 0677. Helplines are open 3pm-8pm Monday to Friday. Alternatively, you can try the one-to-one webchat.
Topics: Health, Real Life, True Life, UK News, Mental Health